 By Anna Evenosky, Guest Blogger
By Anna Evenosky, Guest Blogger
Rewind to that time that is so vague in my head that I can barely remember it. The time of my life when I was as free as a bird spreading its wings for the first time. The time of my life when I didn’t know CRPS existed.
I can’t recall what being pain free feels like. Although, I can recall the happy times I would be lying if I said I didn’t miss. Going from a life where my biggest worries were passing a class, or getting something done on time, to a life of chronic illness, was an adjustment to say the least. Something I wasn’t exactly ready to take on. Although, I’m sure at no point is anybody ready to handle watching their life seemingly crumble to pieces.
Reflecting on my life before Chronic Illness is something I do more often than not. I always find myself coming to the same conclusion and same regret – why didn’t I appreciate how good I truly had it? Why is it that we don’t know what we have until it’s gone. No matter how many people claim that they don’t take for granted being able to walk from point A to point B, truth is they don’t know anything different to be able to appreciate it. To those people who wake up every morning and complain that they are “too tired” to get out of bed. I hope you appreciate that on top of fatigue you don’t need to deal with pain worse than child birth, swollen limbs, and wondering if your body will give out on you when you stand.
Surviving in a life with CRPS is something that nobody should need to face. To those Warriors who have no choice but to fight, I hope I can convince you to always live your life in the moment. Every Warrior deserves to live as “normal” of a life as possible. In fact you’re so busy fighting, worrying, thinking about the future all the time, that sometimes you must learn to let it all go and do what makes you happy. Life is too short and our ‘good days’ are too short to waste them on things that don’t ultimately leave a smile on our faces at the end of the day.
On that rare occasion where you have enough energy and feel well enough to go out with some friends or your family, but you’re torn on what to do, because you have a test in school tomorrow, or have been struggling with too much on your plate at work and should really work overtime, do yourself a favor. Live in the moment. Realize that not getting that A+ won’t make a huge impact on your grade; and realize that you avoiding your work for one more day won’t make a huge difference. Don’t think about what impact this decision will have in the days, weeks, months to come because chances are it has no impact that far into the future. Sometimes, we must stop striving to go above and beyond in everything we do, but shift our focus on making ourselves happy. I’m not saying school and work shouldn’t be a priority. I’m simply stating that your overall well-being and happiness should be just as important. Sometimes it isn’t even a matter of choosing between one or the other, but a matter of finding a happy medium. When a good opportunity comes your way, no matter the sacrifice you may have to make if it’s going to bring you happiness jump at it. You never know when your health may take a turn for the worse and that opportunity may no longer be available to you.
You, a CRPS Warrior, go through and have lost too much to lose your happiness too. Maybe there is no pill we can take or treatment to cure us, but I can assure you that happiness can go a long way and make this life you live a whole lot easier. This is one thing that you can do to truly help yourself. So next time you say “What if?” or “I can’t, I have a lot of work” or “I wish I could, but I really should _______” , smack some sense into yourself and treat yourself to something you deserve. Never lose touch with what brings you true happiness. After all, we never know what the future may bring and I’m sure you would hate to look back at your life and have regrets. Live in the moment it truly is the best medicine you can give yourself.

 By Ryan Ferrell for the RSDSA website.
By Ryan Ferrell for the RSDSA website. Written by Melissa Lovitz, Guest Blogger for RSDSA
Written by Melissa Lovitz, Guest Blogger for RSDSA By Autumn Strand, Guest Blogger for RSDSA
By Autumn Strand, Guest Blogger for RSDSA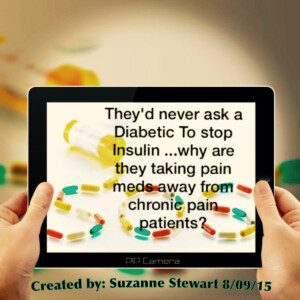 By Suzanne Stewart, author of “
By Suzanne Stewart, author of “