 By Guest Blogger Lara Santoro, Ph.D.
By Guest Blogger Lara Santoro, Ph.D.
Lana Edwards Santoro, Ph.D., is a teacher, educational consultant, writer, and amateur photographer. She also lives with Complex Regional Pain Syndrome (CRPS). Embracing CRPS turned this teacher back into a student.
Lana’s interest in education began when she was in elementary school. She loved reading and never passed an opportunity to visit books in the library. She remembers setting up a “school” at home in her living room, and how her grandfather lovingly subjected himself to her improvised reading lessons. Lana’s early interest in teaching and learning became her professional work. With an interest in multidisciplinary, integrated approaches to education and health, she taught in a residential treatment program, psychiatric hospital, and a center for children and adults with medically complex, developmental and intellectual disabilities.
Lana continued her work in education and obtained advanced degrees in special education and research. She taught pre-service teachers at the undergraduate and graduate level, consulted with state, local, and private agencies on a variety of projects, and presented extensively about how to apply research-based, instructional strategies in the classroom. Lana also served as principal investigator on a series of federally-funded research studies on comprehension where she and her colleagues developed a widely-used intervention and curriculum for struggling readers.
A 2006 tennis match led to a ruptured gastrocnemius muscle, dozens of visits to medical professionals, and—four years later—a CRPS diagnosis. As someone dedicated to “what the research says” about best practices in education, she was overwhelmed by the lack of research for CRPS at the time. She was haunted by what seemed missing, and the research questions that weren’t being asked. Struggling to sort through what was known and not known, Lana became a student again as she applied her interest in education to her experience with CRPS. CRPS became an excuse, of sorts, to return to the library (or, more frequently these days, Amazon.com) to read what she could find on pain management, treatment, and mindful living. Those hours of study culminated in the development of her personal CRPS management curriculum. Because best practice suggests an individualized, multi-disciplinary approach to CRPS treatment, some of the main components of Lana’s management have included:
- collaboration with her medical team on appropriate interventions,
- on-going work with a personal trainer to design and implement a physical training program, (e.g., the application of graded motor imagery strategies and principles of explicit instruction—including the use of models/demonstrations, scaffolding, and strategic integration), and
- the use of a variety of self-management strategies to support daily living (e.g., the University of Massachusetts Medical Center’s Mindfulness-based Stress Reduction program by Jon Kabat-Zinn and Open-focused Training by Les Fehmi and Jim Robbins).
Lana currently works part time from her home in Alexandria, Virginia as a Research Associate and Curriculum Developer with the Center on Teaching and Learning at the University of Oregon. She continues her consultation with local and state education agencies and loves working with in-service teachers. In honor of CRPS Awareness Month, Lana is excited to share some lessons learned and a few strategies from her CRPS management toolkit:
| My Self-Management Toolkit Lana Edwards SantoroAs those with a CRPS diagnosis know, nothing prepares you for CRPS. When I first received my diagnosis, I looked everywhere for a roadmap. I searched all kinds of sources for information that would tell me what to do, what steps to take. I knew that I didn’t want to just live with CRPS. I wanted to be living with CRPS in a full, active way–regardless of whether I was using a wheelchair, crutches, walking without assistance, sitting in a hospital waiting room, spending time in bed recovering from a flare, or enjoying activities with my family.I’ve often viewed my professional life with two distinct emphases: practitioner and researcher. In many ways, my experience has required me to draw fully from both–the research and the application to practice. Here are a few of the “research-to-practice” lessons I’ve discovered on my CRPS journey: 1. Take a research-based approach to CRPS management. To the greatest extent possible, use research on CRPS to guide treatment and self-management decisions. Since research on CRPS continues to evolve, I admit to shamelessly borrowing research-based strategies from other related disciplines. For example, while not entirely specific to a CRPS population, there are research-based strategies that can be applied and adapted from the literature on chronic pain and illness. I’ve also incorporated research on resilience, coping, mindfulness, healing spaces, special education, and neuroplasticity to inform how I approach self-management.
Also, think about how a favorite hobby, like gardening, woodworking, word study, listening to music (without other distractions), or photography, could be used to help with coping. In other words, give yourself a learning project, see how it might apply to living with CRPS, and “geek-out.” (Here’s a note that my reading comprehension research-self would like to share: This self-study approach to CRPS builds comprehension and can add layers of meaning to your CRPS experience. Our ability to cope with difficult challenges often improves when we find ways to connect more meaningfully.)
3. Create your own individualized action plan. Create an action plan just like someone in education might develop an individualized education plan (IEP) for a student receiving special education. Your action plan should be dynamic and evolving. Around the time of my diagnosis, my action plan initially focused on medical intervention and the physical training work required to help me transition from wheelchair use to walking. Currently, my action plan has more of a functional restoration focus and emphasizes activities of daily living (I admit that if I take the time to write things down, I’m more likely to follow my plan and even meet some of my envisioned goals).
4. Pay attention to pain like you are carefully reading a complex text. I find working with pain is a little like reading comprehension. It requires ongoing attention and interaction. I’ve learned that paying attention to subtle details, hard-to-ignore themes, and changes in what the “pain story” communicates overtime, helps me manage and work with pain (somewhat) better. Overall, try to understand and get to know your pain; specifically, learn the micro- or macro-level patterns that cycle through your own “text.”
5. To the greatest extent possible, get moving, even if your path toward movement is infinitesimally slow. Even though it might feel counterintuitive from the body’s chronic pain perspective, working on movement has an eventual pain management payoff. Of course, there are many other benefits to movement too.
6. View CRPS challenges from different perspectives. My photography hobby has taught me the important practice of perspective shifting and re-framing the same shot from different angles. Re-framing allowed me to experience the joy of movement in my wheelchair. As I continue to improve my walking skills, I’ve yet to experience the fluidity, agility, and opportunities for self-initiated acceleration and speed that I learned to appreciate when I went wheeling.
7. Incorporate less as more when scheduling. Many others living with CRPS discuss the importance of pacing and careful scheduling too. I’ll add my voice to this chorus. Like many of you, I admit I can be an over-doer. Learning to be mindful of my body, and the potential subtilties and dynamics of underlying pain (see #3), help me pace within my optimal range of functioning.
8. Change. One of my hardest lessons was learning that I had to open to how CRPS would change my life. When I figured out that I couldn’t continue to do the same things in the same way (ranging from small daily tasks to my job in academia), I started to make the time consuming, and often very difficult, “all in” changes to my schedule and daily routines. When I started to make these changes, and adhered to my new routines, I discovered gradual improvements in my overall functioning. I also learned the profound lesson that change often signals that you’re heading on the path to acceptance.
9. Return to “the library,” whether brick-and-mortar or virtual, and use stories of hope to help chart your CRPS journey. When I first received my CRPS diagnosis, I read, watched, and listened to every story of hope I could get my hands on. I wanted to know how other people lived with CRPS, and how others with chronic illness faced challenges and celebrated life. What I learned from other stories of hope gave me my roadmap for how I wanted to approach life with CRPS. In their wide-ranging perspectives and diversity, these stories are great teachers for how to live resiliently (as a start, read any Linda Lang essay written for RSDSA, if you haven’t already).
10. While I try to take a proactive, positive approach to my self-management, the reality of living with CRPS dictates that pain is an inescapable part of the trip. Simply put, despite Lessons #1-9, we know a CRPS journey can be miserable, exhaustingly disheartening, and even tragic. Just like any hero’s journey, there’s time spent with darkness. Therefore, look for the darkness, pain, and struggle in stories of hope -those themes can equally inform your roadmap. To me, stories of hope aren’t always glossy, or about a victory, or a cure in the traditional sense. Rather, the best stories often highlight the simultaneous acceptance of limitations and determination to overcome them. These narratives are fundamentally about the struggles and setbacks that lead to compassion, enrichment, and complex perspectives. I especially look to others who were diagnosed with CRPS at earlier times when less was known about treatment. Here I find hope through remarkable courage and raw authenticity. |

 Written by Guest Blogger Allison Wells, MD
Written by Guest Blogger Allison Wells, MD Written by Samantha Anderson
Written by Samantha Anderson Written by Samantha Anderson
Written by Samantha Anderson By Samantha Anderson, Special Events Coordinator
By Samantha Anderson, Special Events Coordinator Written by Guest Blogger Gabe King
Written by Guest Blogger Gabe King Written by Guest Blogger Emily S. Nunez
Written by Guest Blogger Emily S. Nunez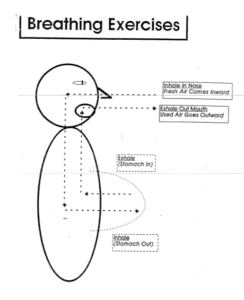 By Guest Blogger Emily Salser Nunez
By Guest Blogger Emily Salser Nunez Written by Tatiana for the RSDSA blog.
Written by Tatiana for the RSDSA blog.