Written by Dr. Katinka van der Merwe for the RSDSA blog.

The Spero Clinic has gained a reputation for effective, non-invasive nervous system rehabilitation, and for the sheer number of people who have found remission after going through our program. Often people ask me why our clinic is so unique in its approach. I think the answer is multifaceted, but certainly, one of the factors that makes us most successful where other approaches have failed is that we approach the body as a whole. This may seem simple, but if you think about it, it is very powerful. When patients are suffering from conditions like CRPS or EDS (Ehler’s Danlos Syndrome), they are often bounced around from specialist to specialist. Each doctor only studies the specific symptomatic area that falls within their specific specialty. They do not consider (or may not have knowledge of) how a condition like CRPS may affect multiple systems. They do not consider the root of the diagnosis, but rather focus on the various symptom(s) they specialize in.
The autonomic nervous system is a control system within your peripheral and sensory nervous system that influences the function of internal organs. This system acts largely automatically without any conscious input from you, and regulates bodily functions such as digestion, sexual arousal, respiration, heart rate, blood pressure, and urination, to name a few. Certain reflex actions such as sneezing, coughing, and vomiting are also controlled by the autonomic nervous system. Within the brain, the autonomic nervous system is controlled by the hypothalamus. The hypothalamus is located just above the brain stem within the brain.
This system is divided into the sympathetic and parasympathetic nervous system. The sympathetic nervous system is largely responsible for speeding up functions in the body, and is known as the “fight or flight” system. The parasympathetic nervous system is considered the “rest and digest” or “feed and breed” nervous system, and mostly is responsible for slowing functions down inside the body. Think of the sympathetic nervous system as the gas pedal in your car, and of the parasympathetic nervous system as the brake.
Pedal to the Medal or Playing Dead: The Two Things Every Single CRPS Patient’s Nervous System Has in Common
What if your body was an airplane and your pilot is drunk? The autonomic nervous system (sometimes known as the automatic or involuntary nervous system) is incredibly important to your health, as this system is the master control system that runs every single function in your body. Most of these functions require no conscious thought from you. You don’t have to remember to breathe, for example. When you are sitting in an airplane, you don’t have to know exactly what the pilot is doing up there in the cabin. You just trust that he is doing his job and will keep the plane in the air and eventually land it safely. In the case of most CRPS sufferers, the pilot is unfortunately up to all sorts of monkey business, and usually has his hand frozen in the full-throttle position.
The sympathetic and parasympathetic nervous systems have exactly opposite effects on the functions of the body. They essentially work in opposition to each other, but in a way that complements each other. As I said earlier, think of your sympathetic nervous system as the gas pedal, and the parasympathetic nervous system as the brake pedal. The balance between the two is crucial for the perfect function of every cell in your body. While they are both crucial to the car, they cannot be stepped on at the same time. As many CRPS sufferers unfortunately find out firsthand, this is bad news for your health. The golden rule of the autonomic nervous system is that if one system is up, the other system must be down.
In every single CRPS patient, one of two abnormal states exist: the sympathetic nervous system has its pedal to the metal, all the time, or the brain has been stressed for so long that the nervous system plays dead. This is much like an animal which, after fighting for its life, understands that its options have ran out, and so it plays dead in a last ditch effort to survive. This may be the case years before you ever develop CRPS, or your nervous system may be injured resulting in this imbalance when you suffer from the traumatic injury that triggered your CRPS. Sometimes CRPS can even be triggered without a traumatic injury or invasive procedure.
The Sympathetic Nervous System: “Fight or Flight”
This system was designed to help your body fight to stay alive when your survival is being threatened. Think of a caveman in hand-to-paw combat with a saber-toothed tiger. This portion of your nervous system responds very quickly (think zero to ninety in a few seconds), since one usually doesn’t have time to calmly ponder one’s response to a life-threatening situation. When your life is being threatened and your body gets ready to fight in order to ensure its survival, every small bit of energy spent is carefully considered. Nothing is wasted. Energy will be rerouted away from systems that do not concern themselves with short-term survival, to where it can be used more readily to fight an immediate threat. For example, blood will flow away from the digestive tract and skin in order to be rationed out to the lungs and muscles. It is more important under those circumstances to be able to fight using your muscles, and to breathe hard and fast, as your body needs oxygen.
Speaking of oxygen, the bronchioles (small air passages) in the lungs will open up, which allows for more oxygen into the blood. At the same time the heart will beat faster. Another physiological change in the body is that the pupils will dilate, allowing more light to enter the eyes. The adrenal glands on top of the kidneys will pump adrenalin in case you need extra motivation besides fear to fight. It will also make all the sphincters (think of pressure valves) in the body, like the urinary sphincter, contract and close tight.
So why does this affect you? There probably isn’t the equivalent of a saber-toothed tiger chasing you every day. Your brain cannot distinguish fear and stress from actual life-threatening situations. Additionally, a very old traumatic event can run in a continuous “loop” in the subconscious mind. The brain cannot distinguish between this old memory and present danger. The old memory almost acts like a computer virus, messing with the software in your nervous system. Your brain does not know that it isn’t happening anymore.
When a person suffers an emotionally traumatic event or a neck injury following, for example, a fall or car accident affecting the brain stem directly or indirectly, the sympathetic nervous system will become overexcited, affecting the whole body. This will cause your sympathetic nervous system, or fight-or-flight response, to be stuck in the “on” position day in and day out—and if your sympathetic nervous system is stuck all the time, your parasympathetic nervous system is turned off. Instead of these two systems working in perfect harmony, the sympathetic nervous system turns into the schoolyard bully, or the puppet master, pulling your body’s strings and directing it on a disastrous course every second of the day. This will create the perfect conditions inside your body that put you at risk to develop CRPS and other autonomic dysfunction or WAD (whiplash-associated dysfunctions). I will discuss each symptom in detail, after we explain how the parasympathetic nervous system works.
The Parasympathetic Nervous System: “Rest and digest” or “Feed and breed”
Think of your parasympathetic nervous system as the system that calms you down, helps you to rest and sleep, helps to facilitate healing in the body, and deals with sexual arousal. It functions to counter the sympathetic system. After a crisis or danger has passed, this system helps to calm the body. Your heart and breathing rates slow, your digestion resumes, your pupils contract, and you stop sweating.
This system will also cause the increase of blood flow to your GI tract following a meal to allow digestion. It stimulates the movements of your intestines (called peristalsis) that move food through your intestines. It will constrict the pupil of the eye, cause you to salivate when appropriate, and is responsible for getting you in the mood for sex. This system, if activated, will activate your immune system, cause increased circulation to the skin and extremities, and help to release your “feel-good” hormones, called endorphins. It will also decrease temperature. It is the main control system that promotes healing. This system is usually underactive, suppressed, or turned off in those who suffer from CRPS. No wonder you are not in the mood for getting frisky!
The Vagus Nerve: Your Severed Lifeline
If you suffer from CRPS, you should familiarize yourself with the vagus nerve, as it is a major player in building the puzzle that forms CRPS. The vagus nerve is the single most important nerve inside the human body outside of the spinal cord. It is one of twelve pairs of cranial nerves. These nerves emerge directly from the brain and brain stem, as opposed to spinal nerves that emerge from the sides of the spinal cord. Each cranial nerve is paired and is present on both sides. The cranial nerves provide motor and sensory information mainly to the structures of the head and neck (think sensations like smell, taste, hearing, or vision, for example.) These nerves are numbered by roman numerals. The vagus nerve is the tenth nerve (CN X), and it is the longest cranial nerve.
Please stick with me here, as I realize that some of you may be bored by the anatomy of the nervous system. I promise that this nerve matters greatly in the development (and therefore also the healing) of the neurological symptoms of CRPS.
The vagus nerve (meaning “wandering nerve”) has multiple branches that diverge from two thick stems rooted in the cerebellum and brain stem that wander to the lowest viscera of your abdomen also connecting to your heart and most major organs along the way, such as the lungs. The vagus nerve supplies motor parasympathetic fibers to all the organs except the adrenal glands, from the neck down to the transverse colon. The vagus nerve is responsible for many different tasks, including (but not limited to): heart rate, digestion, sweating, speech, coughing, fainting, and vomiting, to name but a few. Remember, people who suffer from CRPS also suffer from sympathetic dominance (the schoolyard bully), causing the parasympathetic nervous system to be suppressed and to shut down. This means that people who suffer from CRPS also suffer, by definition, from an underactive vagus nerve.
Just to recap: the parasympathetic nervous system is responsible (in general) for slowing and calming things down, as well as healing and sleep. The vagus nerve forms an electric circuit that links our heart, digestive tract, and lungs to the brain. Let’s look at how this nerve affects specific organs just a bit closer.
Because of the vagus nerve malfunction, CRPS patients almost universally will exhibit some form of GI symptoms or conditions. These symptoms may be as mild as constipation or as severe as gastroparesis, a complete shutdown of the GI system. Other diagnoses may include IBS (irritable bowel syndrome), diverticulitis, celiac disease, Crohn’s disease and gluten intolerance, to name but a few.
In my experience, few doctors will treat these problems as a central nervous system dysfunction. It is far more likely that these patients will be prescribed medicine to counteract their symptoms. If they experience heartburn, they will be given antacids. If they are constipated, they will be prescribed medication for that. Of course, this complicates the toxic load your GI system is already dealing with, not to mention your liver and kidneys.
The following may cause digestive symptoms (especially in patients suffering from CRPS):
- Autonomic (parasympathetic) nervous system dysfunction, turning “off” digestion and the immune system in the gut, specifically malfunction of the vagus nerve
- Overuse of antibiotics causing an imbalance in good versus bad bacteria
- Candida overgrowth resulting from a weakened immune system, heavy-metal toxicity, or not enough good bacteria in the gut
- A poor diet low in fiber, acidic in nature, and high in sugar and saturated fats
- Medications adversely affecting the gut
- Weakened digestive enzymes, resulting in food not being completely digested
- Food sensitivities or allergies
The health of your digestive system is directly linked to the health of your immune system. Almost 70 percent of the immune system resides in your intestinal tract. This branch of the immune system, made up of billions of friendly bacteria and yeast, is responsible for many functions including proper nutrient absorption, production of vital nutrients (produced by the bacteria in your gut), detoxification and alkalization of the body, and last but not least, one of the main weapons your body uses in fighting against bad bacteria.
While we do not have the luxury of space to discuss every digestive problem or diagnosis in detail, we feel strongly that the digestive system of every patient suffering from fibromyalgia must be treated as if it is not well.
The Basic Steps Necessary to Heal the Digestive System
- Detoxify
- Avoid foods that you are allergic to (or get treated for your specific allergies)
- Change your diet
- Rebuild the gut with good food and good bacteria
- Nourish the body with healthy and proper vitamins, minerals, and supplements
In my previous post on the RSDSA blog, I discussed the role that viral and and/or bacterial infections play in CRPS. These infections can wreak havoc on GI track and can also use the Vagus Nerve as a ladder, essentially reaching the brain and causing massive central nervous system inflammation and dysfunction.
It is my experience that the vast majority of CRPS patients also suffer from GI dysfunction. Doctors must recognize this and stop treating the symptoms of CRPS without addressing the underlying nervous system dysfunction.
Dr. Katinka van der Merwe is founder and CEO of The Spero Clinic and practices in Fayetteville, Arkansas with four other chiropractors and a growing dedicated team of twenty staff members. She has gained a reputation of taking on hopeless and severe patient cases and has gained international attention due to her unprecedented success rates in these cases. She treats patients from all over the world, using her Neurologic Recovery Program, the emphasis of which is Neurologic Rehabilitation and restoring balance to the Autonomic Nervous System. She is the author of two books, “Taming the Beast: A Guide to Conquering Fibromyalgia” and “Putting Out the Fire: New Hope for CRPS,” available on Amazon. She is also featured in the newly released best-selling book “Wakeup: Miracles of Healing from Around the World.” In October 2018, Dr. Katinka was awarded Global Chiropractor of the Year in Atlanta, Georgia by the Masters Circle Global for her outstanding achievement in her profession.
Please consider making a donation to RSDSA today!
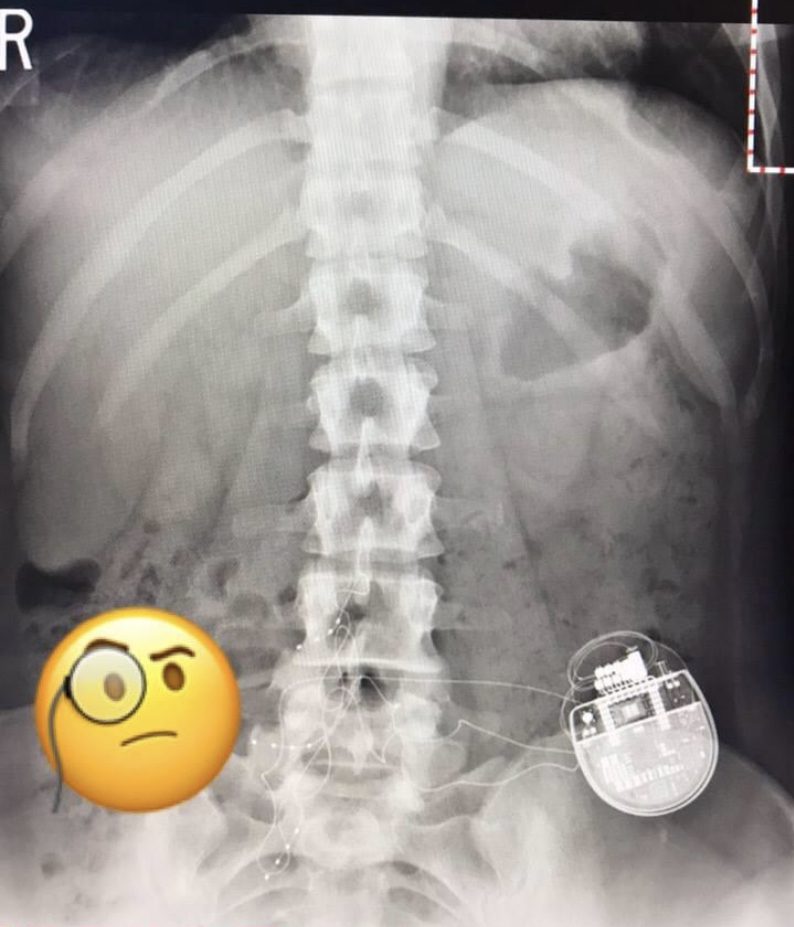
 In August of 2015, I was working as a nurse in emergency transport for Children’s Hospital of Philadelphia. During a call, I rolled my ankle coming off the helicopter. I went to urgent care after my shift and was diagnosed with a sprain after the s-ray was misread (my talus bone in my ankle was actually fractured). From August to April, I saw multiple doctors and completed six weeks of physical therapy on a broken bone, unknowingly. In April, I met with a specialist and after multiple images it was determined my talus was broken, a ligament was shredded, and both tendons were torn. I had surgery in June which included a fibular groove deepening. During the surgery, my sural nerve (a sympathetic nerve) was accidentally cut through but the surgeon failed to inform me with the thoughts that it “would get better.”
In August of 2015, I was working as a nurse in emergency transport for Children’s Hospital of Philadelphia. During a call, I rolled my ankle coming off the helicopter. I went to urgent care after my shift and was diagnosed with a sprain after the s-ray was misread (my talus bone in my ankle was actually fractured). From August to April, I saw multiple doctors and completed six weeks of physical therapy on a broken bone, unknowingly. In April, I met with a specialist and after multiple images it was determined my talus was broken, a ligament was shredded, and both tendons were torn. I had surgery in June which included a fibular groove deepening. During the surgery, my sural nerve (a sympathetic nerve) was accidentally cut through but the surgeon failed to inform me with the thoughts that it “would get better.”


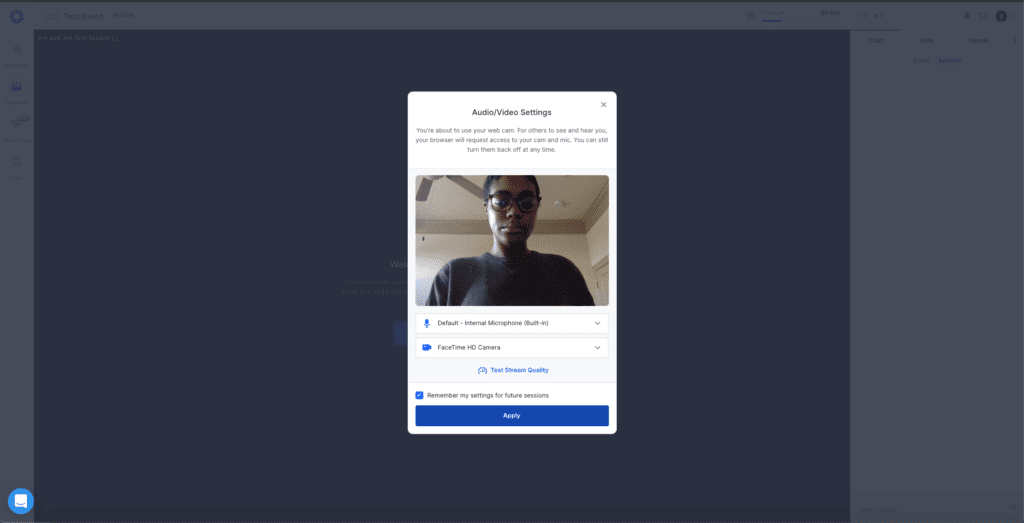
 The RSDSA team is excited to have you join our first virtual conference from October 19th through October 22nd. Below are a few FAQs to ensure you have an amazing experience!
The RSDSA team is excited to have you join our first virtual conference from October 19th through October 22nd. Below are a few FAQs to ensure you have an amazing experience!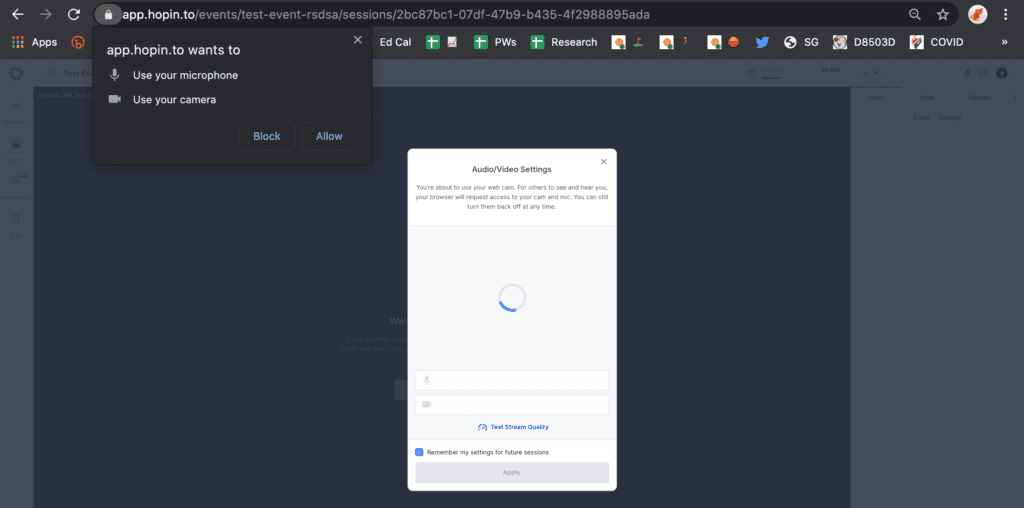


 The last five months have been hard on everyone as we deal with the impacts of COVID-19 in our society.
The last five months have been hard on everyone as we deal with the impacts of COVID-19 in our society.

